Greater Trochanteric Bursitis & Ischial Gluteal Bursitis (What is Bursitis?)
WHAT IS BURSITIS? WHAT IS BURSITIS OF THE HIP?
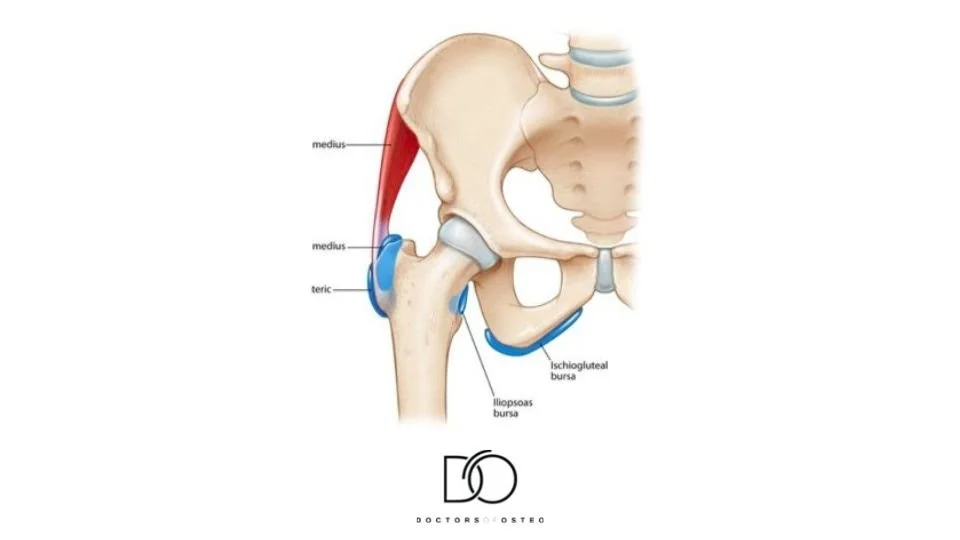
A bursa is a fluid-filled cushion used by the body to lubricate joints and reduce the friction caused by tendon rubbing over bone.
There are bursas throughout all joints in the body. The trochanteric bursa is located on the side of your hips and is one of the most susceptible bursae that can become inflamed. Inflammation of the affected bursa is caused by overuse of the tendon resulting in a build-up of friction or prolonged compression of the bursa. Similarly, ischiogluteal bursitis is an inflammation of the fluid-filled sac that is located between the buttock and the back of the thigh. This bursae is less commonly occurring than greater trochanteric and is usually caused by prolonged sitting, more often on hard surfaces.
Bursitis usually disappears after a few days or weeks, however, the pain may be persistent during this time.
Make it stand out
Whatever it is, the way you tell your story online can make all the difference.
WHAT IS THE SYMPTOMS OF TROCHANTERIC BURSITIS & ISCHIAL GLUTEAL BURSITIS?
- Hip feels achy or stiff
- Painful with movement or when pressing on it
- Swelling
- Redness
HOW DOES GREATER TROCHANTERIC BURSITIS OR ISCHIAL GLUTEAL BURSITIS OCCUR?
Bursitis can occur due to a multitude of reasons. Some of the most common mechanisms are direct trauma, for example, falling onto the side of your hip or your ischial tuberosity (“sit bones”). Another common mechanism for greater trochanteric bursitis is due to overuse which is common within the sporting population. Ischiogluteal bursitis can also be caused by long periods of sitting, especially on solid surfaces without support.
WHAT SHOULD I AVOID DOING IF I HAVE GREATER TROCHANTERIC BURSITIS OR ISCHIAL GLUTEAL BURSITIS?
- Overload: Try avoiding exercises that cause repetitive use of the hip i.e.cycling, walking, kicking.
- Poor Posture: Try to avoid sitting at your desk for hours on end without a break or standing for hours on end without short breaks.
- Sleeping/ Sitting on affected side: You may want to avoid crossing the leg when sitting on the affected side or sleeping on it as it will further compress the bursa.
DO I HAVE TO HAVE SURGERY FOR GREATER TROCHANTERIC BURSITIS OR ISCHIAL GLUTEAL BURSITIS?
For stubborn bursitis that isn’t responding to more conservative methods, a corticosteroid injection may be trialled. This is a strong anti-inflammatory medication used to decrease the amount of inflammation, and therefore pain. In severe circumstances, a surgeon can arthroscopically remove the bursa through a small incision on the hip, when persistent bursitis is present and all other treatment modalities have failed.
WHAT CAN I DO AT HOME TO TREAT GREATER TROCHANTERIC BURSITIS OR ISCHIAL GLUTEAL BURSITIS?
- Rest/ Ice: Resting the overloaded area and icing when painful.
- Avoid the aggravating activity: Try avoiding the activities that you suspect may cause or contribute to the pain.
- Medication: Non-steroidal Anti-inflammatories (NSAIDs) such as aspirin, ibuprofen and naproxen can reduce the inflammation and pain in the area.
- Exercises and stretching: Your osteopath will be able to identify the muscles that may be weak or too tight and causing the compression of the bursa. They will then prescribe a specific exercises regime to tackle these imbalances.
HOW CAN I PREVENT BURSITIS?
If you have previously had trochanteric or ischiogluteal bursitis, muscle strengthening around the area will decrease the chance of bursitis from reoccurring. Warming up before intense exercise and cooling down afterwards is the most effective way to avoid bursitis and other muscle strains. Taking regular breaks while carrying out activities that involve repetitive movements has also been found beneficial. This will help avoid placing excess strain on one particular joint of your body. An increased BMI (Body Mass Index or “weight-gain”) can have negative effects on your bursa and can also contribute to the presentation of greater trochanteric/ ischiogluteal bursitis.
CAN OSTEOPATHS HELP WITH BURSITIS?
Osteopaths regularly treat bursitis with a range of treatment techniques and lifestyle advice.
● In the initial consultation, your osteopath will assess your hip and may order radiographic imaging to assist with the correct diagnosis, prognosis (tissue healing time) and management plan.
● Osteopaths can help you identify the possible aggravating and contributing factors to the development of your bursitis.
● Osteopaths will use a range of individualised soft-tissue, massage, manipulation, stretching and mobilisation techniques during your 45min appointment to improve pain, swelling and fluid drainage.
● A comprehensive exercise rehabilitation program will be implemented to prevent further deterioration of the hip and to strengthen the appropriate muscles and improve joint mobility.
● An adjunct treatment available to Doctors of Osteo is Shockwave Therapy. A study by Seo et al., 2018, showed immediate benefits in 83.3% of their population after shockwave therapy in patients with greater trochanteric bursitis. 55.6% of their population also reported improvement after 12 sessions of therapy (on average 27 months later) (1)
References
(1) Seo, K. H., Lee, J. Y., Yoon, K., Do, J. G., Park, H. J., Lee, S. Y., Park, Y. S., & Lee, Y. T. (2018). Long-term outcome of low-energy extracorporeal shockwave therapy on gluteal tendinopathy documented by magnetic resonance imaging. PloS one, 13(7), e0197460. https://doi.org/10.1371/journal.pone.0197460
Providing healthcare with our osteopaths near me in Hawthorn, Hawthorn East, Kew, Balwyn, Canterbury, Camberwell, Camberwell East, Richmond, Malvern and Glen Iris.